Providers are required to be resilient and ready to do whatever it takes. Nowadays, it rings truer than ever for Salil Shah, MD. He’s been on the front lines in a COVID unit. For the locums hospitalist at a rural midwestern facility, patients have always come first. “The hospital was well prepared for what might happen,” says Dr. Shah. “To limit overall exposure to COVID-19, physicians work in a negative pressure unit to investigate patients. You treat a patient as COVID- positive until proven otherwise.” Over the last several months, the protocols have changed in the hospital, according to Shah. “The hospital has been extremely vigilant,” he asserts. “There is a daily temperature check for staff and all employees stay masked up and wear a face shield with every encounter.”
The hospital’s PPE includes portable air purifying respirators (PAPR). Shah says he worked four weeks over two months in the COVID unit. “It was not overwhelming, but it was stressful. The [patient] burden here is low compared to metropolitan areas because the area is geographically distant from a major city, which could be more susceptible to the pandemic,” he says. “This hospital has done an excellent job handling the pandemic and is prepared for any potential of another surge.”
Patients Return for Non-Essential Surgeries and More
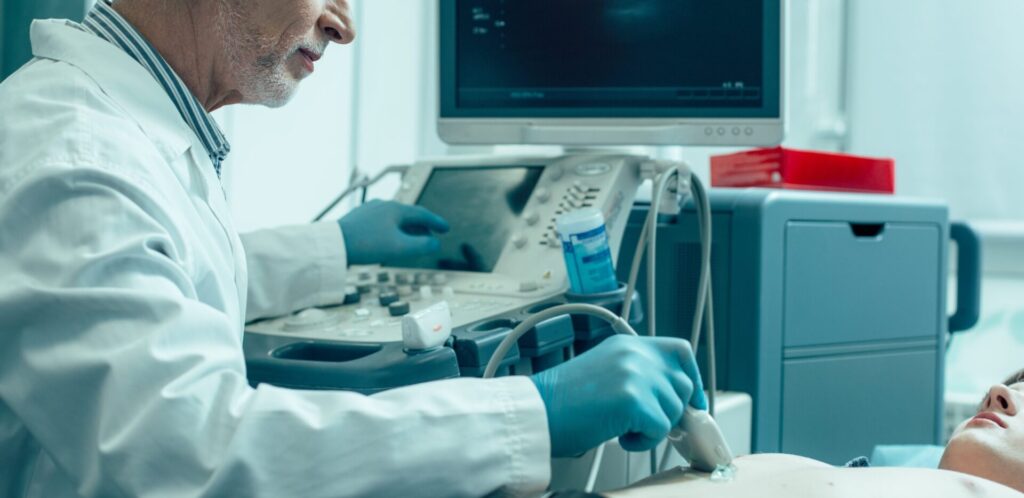
While patient volume fell off at the start of the Coronavirus, Shah reports that patient volume has since gone up. “Non-essential procedures have resumed, and as always, hospitalists are consulted. Acute exacerbations of chronic diseases will always be there,” says Shah. “As an internist/hospitalist, this is our ‘bread and butter.’ Volume has picked up at my facility with heart failure exacerbations and COPD exacerbations, sepsis, acute kidney injuries (chronic kidney disease), liver failure and the like. Interestingly, I have encountered a surge in alcohol withdrawal syndrome and other complications from alcohol during this [pandemic] period. “
The Locums Path
Shah’s career is locums centric. He is a self-described “Locum Tenens Hospitalist.” Since graduating as a Resident Physician at Tallahassee Memorial Hospital in 2017, after earning his Doctor of Medicine degree from Ross University Medical School, he sought maximum flexibility that would allow him to do what he wanted. That not only meant a chance to travel, but locums jobs have also given him the opportunity to be his own boss as an independent contractor.
Of equal importance to work-life balance, locums has provided him with the ability to see how medicine is practiced at different facilities. The hospital environment he is currently in is physician centered with a CEO who is a physician at the helm, rather than a corporate MBA at the top, says Shah. “There is a high retention rate here. Employees are bonded and have a satisfaction level that is better than anywhere I have worked.”
Locums and COVID-19
Shah travels to his home base on his week off. “Support has been great from Hayes, especially with travel during this pandemic,” he says. “The team gets back to me with answers promptly, even after hours.” Speaking from first-hand experience, he admits that travel is different now. “Empty airports and staying in hotels have been interesting.” But for Shah, everything about this locums assignment works: “Twenty shifts a month, two weeks on, one week off. My typical rounding list is on average 15 patients and that is split with a PA. It’s a 10-hour shift with no ICU work, and with much lower stress in a reasonable working environment.”
Whether he returns to the COVID unit depends on scheduling. “I’m not sure if I will be in the COVID unit again, but I am ready to serve if called upon.”