Heart disease has been the leading cause of death in the United States since the 1950s. But while we’ve made huge advances in cardiological medicine, the impact of those advances is now being threatened by physician shortages. Here’s how physician shortages are impacting cardiovascular care—and what physicians can do about it.
The Supply and Demand Imbalance at the Heart of Cardiology
At its core, the cardiologist shortage has many of the same causes as the general physician shortage: barriers to entry, including medical school debt and years of training, lack of work-life balance, and increasing administrative work—which also contributes to burnout, a major driver in physician shortages in and of itself.
All of these pressures are decreasing supply at a time when demand for cardiologists is higher than ever, given the aging patient population and the increasing rates of chronic heart disease. Chronic heart disease rates have doubled in the past two decades—and yet according to an American Heart Association Journal study, less than half of American counties have a practicing cardiologist.
This impact is felt particularly hard in rural communities. 86.2% of rural counties have no cardiologists, according to a study by the Journal of the American College of Cardiology. That same study found that in counties without cardiologists, patients were having to travel, on average, over 80 miles to access cardiac care.
This lack of access has a major impact on patient outcomes: both the AHA and ACC studies show that counties without a practicing cardiologist showed significantly higher mortality rates from heart disease.
Physician Shortage’s Impact on Preventative Cardiovascular Care
According to the American College of Cardiology’s Task Force on the Cardiovascular Workforce, the physician shortage is hitting general cardiology the hardest—which means that it’s having a significant impact on the kind of preventative care that is crucial to catching heart disease early and improving patient outcomes.
ACC’s task force reports that many cardiology fellows go on to subspecialty training—partially due to the fact that these specialties often pay at higher rates. Given the increasing complexity of cardiology, specialists have an important role to play—but the trend toward hyperspecialization means that there aren’t enough general cardiologists to perform initial testing and diagnosis.
As a result of these shortages, wait times have increased by over 25% for general cardiovascular visits since 2017, with patients waiting nearly a month on average to see a cardiologist. Since many heart diseases depend on early detection and treatment, this means that patients at the beginning of their cardiac care journey are increasingly unable to access care.
We are seeing the results of this lack of care in mortality numbers: heart failure mortality is on the rise, with a significant increase in heart failure deaths among younger adults. And according to the JACC’s 2026 Cardiovascular Statistics Report, hypertension-related cardiovascular death rates have nearly doubled in the past two decades, while treatment rates have plateaued.
Filling Gaps in Cardio Care with Locum Tenens
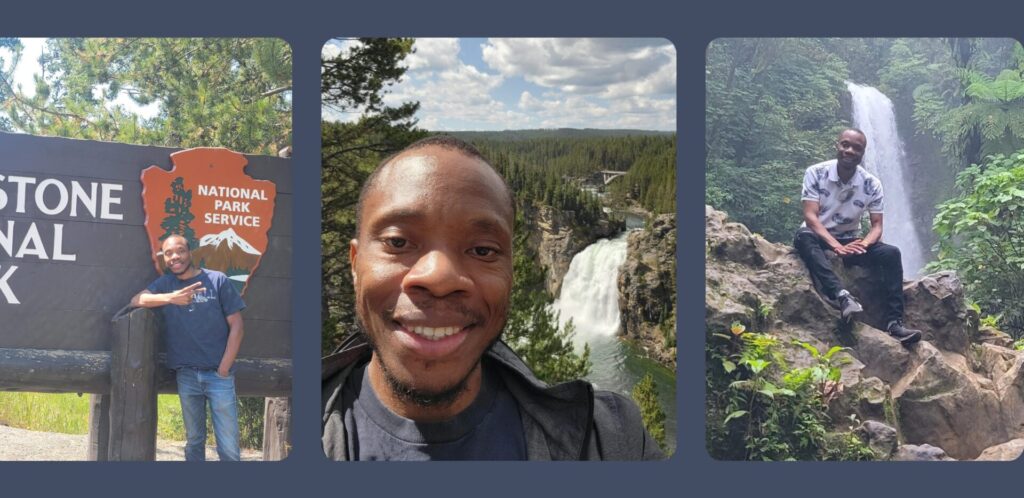
While the cardiologist shortage isn’t going away anytime soon, locum tenens provides a way for physicians to have an impact on patient outcomes, especially in rural areas. Locums allows physicians to make a difference by bringing their skill set to facilities and communities that have been most impacted by the growing scarcity of cardiologists.
“Having a locums cardiologist in these communities makes a huge difference,” said Dr. Marc Atzenhoefer, a cardiologist who works as a locum at a South Dakota critical access clinic.
“Because we know when somebody has critical aortic stenosis, their mortality rate is 50% within one year. By year three, they’re gone. So if there’s no one in these critical access areas listening to peoples’ hearts, picking up on that murmur, identifying what it is, and getting them the care they need, then they are looking at two years of life, tops.”
Dr. Atzenhoefer would know: as a locums cardiologist, he was able to catch a critical aortic stenosis using only his stethoscope, because his South Dakota clinic didn’t have an echo. “That’s not something I could do until I had the opportunity,” said Dr. Atzenhoefer. “But I was able to catch it, and I was able to give that patient a new heart valve. It was amazing.”
With locum tenens, you’re able to take the skills you honed through years of practice, and bring them to communities who desperately need cardiac care. And that impact goes a long way in making physicians feel fulfilled in their work. “Locum tenens gives you the opportunity to challenge yourself and to make a difference,” said Dr. Atzenhoefer.